AgentHack submission type
Agentic UI Automation
Name
Mamta Bagde
Team name
CogniCare
Team members
How many agents do you use
Multiple agents
Industry category in which use case would best fit in (Select up to 2 industries)
Finance
Healthcare Pharma
Complexity level
Advanced
Summary (abstract)
The Agentic Automation - Denial Categorization & Appeal Letter Submission is an AI-powered automation solution that simplified the denial management process in Healthcare Revenue Cycle Management. It combines AI, RPA, and human-in-the-loop validation to analyze denial reports, classify denial reasons, draft appeal letters, and track outcomes.
The agent reads denial reports and uses the given context on mapping of codes (Denial Codes, Claim Adjustment Reason Codes, Remittance advice remark codes, Procedure Codes), it analyzes, categorizes, and recommends actions. It classifies denials into Eligibility, Coding Errors, Missing Documentation, and suggests recommended action.
Detailed problem statement
The current denial categorization and appeal preparation system is manual, inefficient, and reactive, leading to revenue leakage, delayed responses, and inconsistent outputs. There’s a pressing need to adopt agentic automation that not only improves the process but also enhances accuracy, speed, and strategic decision-making, all while preserving human oversight where it’s required.
In the existing system, denial categorization and appeal preparation process are largely manual, heavily relying on staff to review denial reports, interpret complex medical and billing codes, and prepare appeals accordingly. Each denial report X12 835 files are analyzed using Denial Codes, Claim Adjustment Reason Codes (CARCs), Remittance Advice Remark Codes (RARCs), and Procedure Codes. Staff are responsible for identifying the denial category (e.g., Eligibility, Coding Errors, Missing Documentation) and determining the appropriate course of action, such as appeal, resubmission, or escalation.
End-to-end processing of a single denial report manually can take anywhere from 2 to 48 hours. A team of 12 handles approximately 700-800 denial reports per month, making the process highly time-intensive process that significantly contributes to staff burnout.
• Denial management remains a highly manual process involving multiple teams, including billing, appeals, and revenue cycle analysts.
• Staff must interpret payer responses, extract adjustment and denial codes from X12 835 files, and determine next actions manually.
Challenges in the Current System:
- Revenue Loss Due and delayed revenue recovery:
Every missed or delayed appeal translates directly into lost revenue, as timelines for payer responses are often strict. The combination of delays and inefficiencies contributes to increased write-offs and staff fatigue. - Staff Fatigue and Inefficiency:
Repetitive and manual denial processing tasks lead to employee fatigue, lower productivity, and increased risk of burnout. Manual workflows also slow down the overall revenue cycle. - Manual decision-making bottlenecks: Determining appeal strategies still relies heavily on human input, slowing resolution.
Detailed solution
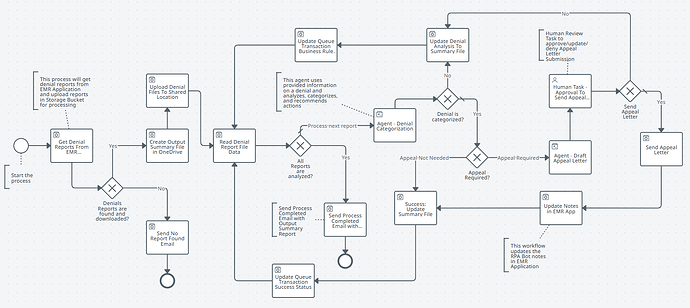
This solution reads and analyzes uploaded denial reports, classifies the type of denial, and drafts appeal letters if applicable. A human reviewer verifies the appeal via UiPath Action Center before the bot sends it to the payer. A detailed summary sheet is maintained for reporting. Technologies used include Agents, Maestro, AI, UiPath RPA, and Action Center.
Steps:
-
Download Denial Reports from CogniCare EMR (Electronic Medical Record - Application created for Demo recording) Application and upload the Denial Reports to Shared Location OneDrive
-
Performs Report Data Analysis to identify Denial Code, Denial Reason, is appeal required, Billed Amount, Allowed Amount, Claim Number, Member ID, Payer Information, Healthcare Provider Information, etc.,
-
Denial Categorization: Classify denials into predefined categories based on denial codes and descriptions. Categories include:
a) Eligibility Issue
b) Coding Error
c) Medical Necessity Denial
d) Authorization Issue
e) Missing Documentation -
Root Cause Analysis & Suggested Actions
-
If Appeal is needed, then draft Appeal Letter.
-
Send Appeal Letter for Human Validation before sending
-
Report Generation - Summary File
-
Updated Bot Notes in EMR Application
-
Send Output Summary Report via email to Business/SMEs
Demo Video
Expected impact of this automation
- Using Agentic Automation, one denial report can process under 2-3 minute
- End-to-end processing of a single denial report manually can take anywhere from 2 to 48 hours.
- 80-90% reduction in manual handling time
- Reduces manual effort and speeds up appeal preparation.
- Prevents lost revenue due to missed or delayed appeals.
- Enhances visibility with a detailed summary output.
UiPath products used (select up to 4 items)
UiPath Apps
UiPath Integration Service
UiPath Maestro
UiPath Studio Web
Automation Applications
EMR Application (Created for demo purpose), Integration Services Microsoft Outlook 365, Microsoft OneDrive & SharePoint
Integration with external technologies
Open AI - GPT-4o-2024-11-20
Agentic solution architecture (file size up to 4 MB)
Sample inputs and outputs for solution execution
Inputs:
- Sample Denial Reports are downloaded from CogniCare Denial Management Application and uploaded to OneDrive Shared Location.
Note: The app is created for the demo purpose - URL: claim-clarity-central - Summary File Template which will be used by the bot to create Output Summary File. Summary File Template link: Sign in to your account
- Context Grounding - Storage Bucket Files for mapping Denial Codes, Claim Adjustment Reason Codes (CARCs), Remittance Advice Remark Codes (RARCs), and Procedure Codes.
Output:
Agent analyzed output will be saved in the Output Summary File created by the bot in OneDrive Shared Location and emailed it to SMEs (Subject Matter Experts)/Business.
Example: One of the Output Summary File generated by the bot: Sign in to your account